Shin splints and stress fractures are types of injuries commonly experienced by health enthusiasts. Despite their strong association, they are completely different conditions that require specific medical intervention.
Summary Table
| Shin Splint | Stress Fracture |
| Highly attributed to engaging in repetitive activities that pose mechanical stress on the tibia (shinbone) and its surrounding connective tissues | Commonly caused by either a sudden increase in the intensity of physical activities or by repetitive mechanical force |
| Characterized by a tight, radiating pain that runs along several inches of the bone | Characterized by a deep, throbbing pain that affects one or multiple parts of the bone |
| Usually does not cause discomfort during walking, hopping, or other forms of light exercise | Causes discomfort during walking, hopping, or other forms of light exercise |
| Diagnosed through a physical examination | Diagnosed through a bone scan or an MRI |
| May progress to a stress fracture or muscle compartment syndrome | May progress to a complete fracture |
| Requires rest, cold compress, over-the-counter pain medication (when needed), and training modification | Requires cold compress, over-the-counter pain medication (when needed), training modification, and complete rest from running and high impact sports until healed |
Definitions
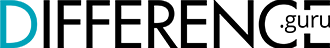
A shin splint, also called medial tibial stress syndrome (MTSS), is a medical condition that involves the inflammation of the tibia – the large bone found in the lower part of the leg.
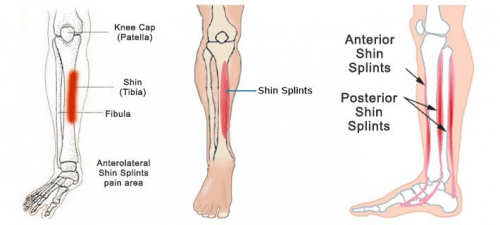
A stress fracture, on the other hand, is a stress-induced bone fracture caused by sudden mechanical force.
Shin Splint vs Stress Fracture
Many people, including athletes and members of the military forces, fail to recognize the difference between shin splints and stress fractures, especially during training. As a guide, below are some of the important factors that draw a line between these two conditions.
Causes
Although there is no direct cause linked to developing a shin splint, it is highly attributed to engaging in repetitive activities that pose mechanical stress on the tibia (shinbone), along with the connective tissues surrounding it. As stress accumulates, the tibia becomes inflamed, causing pain and discomfort.
Stress fracture, by comparison, is commonly caused by either a sudden increase in the intensity of physical activities or by repetitive mechanical force. To adapt to stress and recuperate, the bone normally undergoes “remodeling,” which is a physiological process that destroys and rebuilds bones. However, once the amount of stress undermines the bone’s ability to recover, stress becomes enough to cause a fracture. Similarly, athletes who engage in highly intense sports or activities may also experience stress fracture even if they follow a strict workout regimen. As stress accumulates due to repeated trauma, parts of the bone become susceptible to weakening, which may lead to a stress fracture.
Symptoms
A shin splint and a stress fracture usually affect the lower part of the leg, but there are differences in their level of pain and discomfort. Patients suffering from a shin splint experience a tight, radiating pain that runs along several inches of the bone.The good news: although it causes pain during strenuous activities (i.e. running), it usually does not cause discomfort during walking, hopping, or other forms of light exercise.
A stress fracture, by contrast, causes a deep, throbbing pain that affects one or multiple parts of the bone, and is usually dime-sized. Unlike a shin splint, a stress fracture, depending on the severity, can cause pain even during light exercise or walking. Typically, the lower part of the tibia becomes painful when the foot touches the ground.
Diagnosis
A shin splint is usually diagnosed through a physical examination. If the specialist suspects medical conditions other than a shin splint, patients are advised to undergo an x-ray, a bone scan, or an MRI. Unfortunately, a stress fracture does not always show up on x-ray results, especially if the fracture is too small. In cases like this, specialists prescribe a bone scan or an MRI for confirmation.
Additionally, a shin splint and a stress fracture can be differentiated by a “hop test,” where the patient needs to hop using one foot (the affected limb). If there is no pain upon hopping, the limb may not be affected by a stress fracture. But while this may be applicable in some situations, it’s always best to consult a specialist.
Complications
Between the two, a stress fracture is more alarming as it may progress to a complete fracture – a complete break in the bone that requires surgical treatment. Nonetheless, a shin splint, when mismanaged, can result in either a stress fracture or muscle compartment syndrome, which may cause permanent muscle damage.
Treatment
A shin splint and a stress fracture bear similarities in terms of medical management. They both require rest, cold compress, over-the-counter pain medication (when needed), and training modification. However, stress fracture requires more limitations in movement to prevent injury progression. Usually, athletes need to stop any form of high impact activities (i.e running) for around 6-8 weeks.